Our Services

OPG: (Orthopantonomogram/panoramic dental x-ray) is a 2D image that displays all the teeth, as well as your jaw joints and your sinuses. This imaging is done to make a general assessment of patient’s oral status, or as a record of oral status before and after dental treatment or surgery.

Lateral Ceph: Lateral Cephalometry X-Ray is a 2D image that displays the side profile of your face and jaw. This imaging is done to make an orthodontic or surgical evaluation for treatment planning. Sometimes a PA (posterior-anterior) ceph is requested when there is facial asymmetry, dental crossbites and functional mandibular displacements.
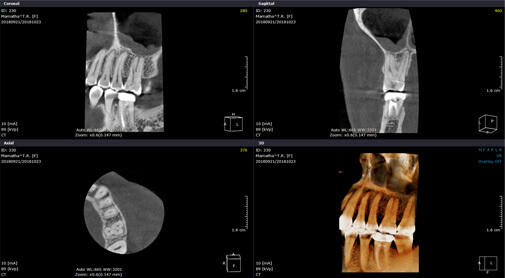
CBCT: Cone Beam Computer Tomography is a 3D CT scan that displays the oral-facial anatomy including the teeth in multiple planes. Clinicians refer this examination to provide them with additional information when previous x-ray examinations are inconclusive, or as a supplement to other x-ray examinations. It is used for surgical procedures, third molar extraction, implant placements, and for endodontic procedures.
Who does the RCT?
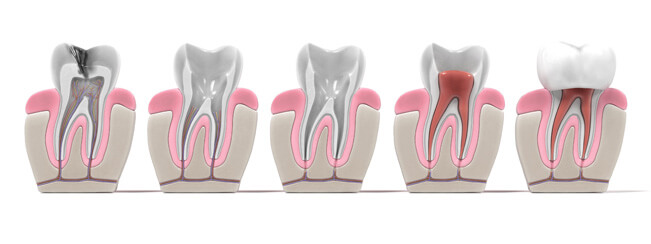
Endodontics is the branch of dentistry concerning dental pulp and tissues surrounding the roots of a tooth. Root canal treatment or endodontic treatment treats the soft pulp tissue inside the tooth. An endodontist is a dentist who specializes in endodontic treatment or root canal treatment. They perform routine as well as difficult and very complex endodontic procedures, including root canal treatment, endodontic surgery and special procedures to save teeth after traumatic dental injuries. Advanced technologies and specialized techniques used by endodontists give them a very accurate view of the inside of the tooth and allow them to treat the tooth quickly and comfortably.
At Mig Dental, RCT is performed in Microscope Enhanced clinical setup which helps in visualization, illumination and also helps to achieve quality work.
After the initial diagnostic tests – both radiographic and clinical – for the problematic tooth, either anterior or posterior, the root canal treatment is planned. Some tooth condition may warrant a CBCT to make an accurate diagnosis and appropriate treatment plan.
Though we do perform single sitting RCT, usually we take two or three sittings (each around 45 minutes) to complete. Pulpal condition plays a vital role in determining the number of visits. We take at least two visits to make sure the patient is infection-and pain-free and clinically comfortable at the finish of the procedure.
If there is abscess or swelling or already failed root canal treatment, multiple visits may be needed, which may go even for months, with intermittent medicament dressings. This clears the infection, aids in appreciable healing both clinically and radiographically and helps to finish the case confidentially. Following the root canal, the tooth is restored with filling (core) material immediately. It the tooth lacks sufficient tooth structure, we place a post inside the root and then place the filling material.
Once the RCT is completed, we recommend placing an appropriate restoration (crown) over the tooth to restore its shape and functionality.
What's the success rate of RCT?
Root canal treatments are successful in over 95% of completed cases. The outcome depends on a wide range of factors, but includes the skill of the dentist; the co-operation of the patient; the anatomy of the patient and access to the tooth; the health, well-being and healing capacity of the patient; the type and quantity of bacteria present in the mouth and in the root-canal system; the shape of the root canals; position and angulation of the tooth; previous restorations of the tooth and pathology associated with the tooth. You will be informed as soon as possible if difficulties are encountered.
When RCT cannot be done or advised?
1. Badly broken teeth which cannot be restored.
2. Some teeth do not respond to RCT, they need to be extracted.
Persistent Infection:
It is possible for bacteria to persist in the bone following root canal treatment for a number of reasons. These include exceptionally virulent, strong bacteria and insufficient healing capacity of the patient. This may result in need of extraction.
Retreatment
Endodontic retreatment treats a tooth that has already had a prior root canal therapy done. There are many varieties of reasons why RCT can fail. A careful examination and diagnosis can determine whether a retreatment or surgical procedure can preserve the tooth or extraction will be necessary.
Root canal treated tooth can fail resulting in pain, swelling or persistent disease. Many times endodontic retreatment or surgery can solve the problem and allow retention of the tooth.
Depending on the case, retreatment can be very successful. But we prefer to start the case only after thorough discussion of the tooth condition, prognosis and consent of the patient.
Apical Surgery
If nonsurgical retreatment is not an option or has failed, then endodontic surgery should be recommended. Endodontic surgery may also be recommended in conjunction with retreatment or as an alternative. This surgery involves making an incision to allow access to the tip of the root.

A dental filling or dental restoration is a treatment to restore the function, form, integrity or missing tooth structure resulting from caries or external trauma.
Depending on the severity, location of the disease and the destruction caused we have different materials and techniques to restore the teeth.
Techniques
Direct Restorations
This technique involves preparing the tooth - that is removing the caries/defect and then placing the material into the prepared cavity. The advantage is it can be placed/done in a single procedure.
Materials
Tooth coloured composites, silver amalgam and cements.
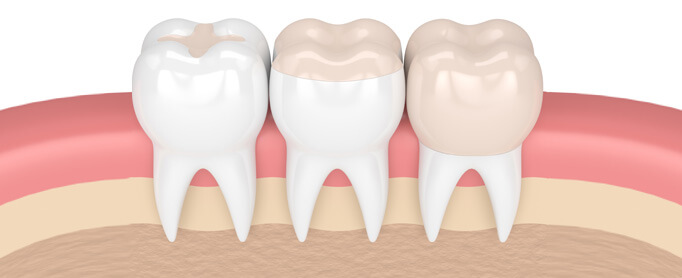
Indirect Restorations
In this technique the restorations are fabricated outside the mouth – in the lab by lab technicians. The cavity/tooth is prepared (removal of disease/defect), then the impressions are taken of the prepared teeth, sent to the lab and the lab technician fabricates the indirect restoration. Then the finished restoration is bonded to the prepared teeth permanently with a dental cement. This needs two visits. In between, the tooth/teeth are temporarily restored.
Materials
Precious metal-gold, non precious metals, composite, ceramics.
For the anterior/front teeth, direct or indirect tooth coloured restorative materials are used.
In the posterior/back teeth, since they need high strength materials, depending on the severity, direct or indirect techniques, metal or teeth coloured restorations are used.
Prosthodontics is the dental specialty that focuses on dental prostheses. Prostheses like dentures, crown and bridges and implants are used to rehabilitate mastication (chewing), improve aesthetics, and aid speech. It can either be fixed permanently or removable prostheses.
A prosthodontist is a dentist who specializes in prosthodontics.
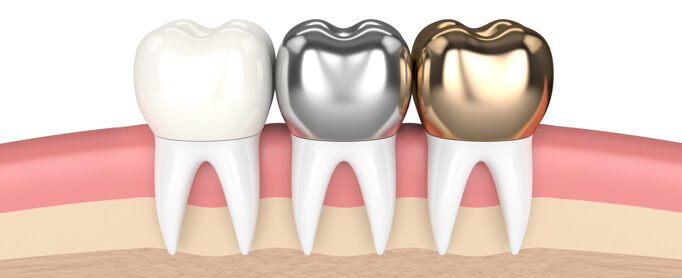
Crown
A dental crown or a cap is also a type of restoration, which completely covers or encircles a tooth or implant. Crowns are done to restore or get back the tooth shape, size, and strength and improve its appearance. Crowns are also used to improve alignment and dental occlusion.
Crowns are recommended:
1. To replace large filling when there isn’t enough tooth structure remaining.
2. To protect weakened tooth structure (caries) from fracturing – because of disease – caries.
3. To restore fractured teeth.
4. To cover poorly shaped or discolored teeth.
5. To protect the tooth that has had root canal treatment.
Choice of materials for crowns
1. Tooth colored
a. Resin based
b. Ceramic-metal with full coverage ceramic
c. All-ceram
2. Metal crowns
a. Gold
b. Chrome-cobalt.
Based on tooth position, bite/occlusion, gum health, cost, the material is advised to the patient.
Procedure
The procedure of fabricating and bonding/cementing the crown needs two appointments. The first appointment involves preparing or shaping the tooth – where the tooth is reduced all around (1mm – 2 mm) depending on the choice of material. Then the impressions are taken and sent to the lab. Then the temporary crown (resin) is made and temporarily cemented. Before the next appointment, dental lab will fabricate the crown.
In the second visit the permanent finished crown will be cemented with adhesive cement.

Bridges
A dental bridge is a fixed dental restoration of one or more missing teeth by joining an artificial tooth to the adjacent tooth or dental implant. Bridges will span the area where the teeth are missing.
When we advise fixed bridges, patient’s expectations will be discussed and thorough patient history will be obtained.
Replacement of missing teeth with fixed bridge may not always be indicated and both patient factors alongside restorative factors will be considered before deciding for bridge.
Materials Used
- Metal
- Tooth colored metal with full coverage ceramics
- All ceram
Number of visits: Usually requires two sittings.
- First visit tooth preparation, impression making. Sometimes, additional visit may be required to check the bite.
- Second visit, the bridge fabricated from the lab will be checked in mouth for the fit and cemented using adhesive cement.
The survival rate of bridge work can be affected by the span of the bridge needed, the proposed bridge, the size, shape and condition of the teeth that will support the bridge. Any disease including caries, periodontal disease will be treated and followed by a period of maintenance to ensure patient compliance in maintaining proper oral hygiene.

Removable Partial Dentures
A removal partial denture (RPD) is a denture for a partially edentulous (missing) patient who desires to have replacement of teeth for function and aesthetic and who cannot have bridge (fixed partial denture).
It is called removable partial denture because patients can remove and reinsert it. They are usually made with metal framework and resin teeth. This needs three or more visits.

Complete Dentures
A complete denture is a removable denture used to replace all the teeth within a jaw. A complete denture is constructed when all the teeth in the arch are missing.
A complete denture can be given to both arches
or
A complete denture can be opposed by natural dentition.
or
A complete denture can be opposed by fixed bridges or partial dentures.
Treatment Duration
Construction of complete denture is a multi-visit procedure (about 5 to 6 visits) that includes patient assessment, primary impressions, secondary impressions, bite registration, Try in, fit and review.
Instructions to complete denture patients
The dentures are custom made and specifically designed and fitted to ones mouth. One will need some time to become accustomed to new dentures. Every set of denture will feel different and a period of adaptation is required where the patient will need to learn how to eat and speak again. The time it takes to adapt to new dentures varies from person to person, and may require weeks to months.
Initially over the first week, it might feel uncomfortable and bulky. Gums may feel sore and might need adjustments. Some patients may have gagging sensation that may slowly subside and some may notice increased saliva in their mouth. Speech may be affected but will improve slowly. Initially there may be some difficulty in eating. Maintain soft diet for the first few weeks, before slowly re-introducing hard foods.
Maintenance
1. Clean the denture after eating every meal. Rinse them under running water or mouth wash to remove any large food debris. Brush all surfaces of denture with a tooth brush or denture brush using soap or other approved denture cleaners. Inadequate cleaning can lead to plaque accumulation – denture sore mouth or fungal infection.
2. Avoid using
a. Hot or boiling water.
b. Tooth pastes as they are often too abrasive
3. Remove the denture every night and soak them in ordinary water or a recommended disinfecting agent. Denture should not be allowed to dry out as it can cause them to shrink. It is also important to allow tissues to recover.
4. Overtime, the patient will experience progressive bone loss underneath your denture because of missing teeth. It is not painful but denture may start to feel loose.
It is recommended that dentures be changed every 6-7 years in order to protect and preserve the remaining oral tissues.
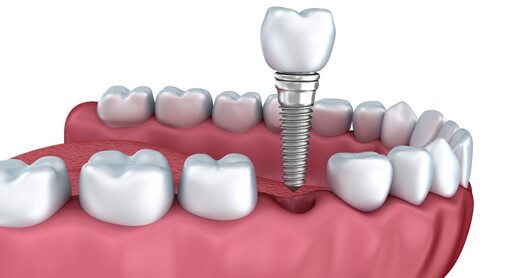
DENTAL IMPLANTS
A dental implant is an artificial tooth root that is placed into your jaw to hold a replacement tooth or bridge. Dental implants may be an option for people who have lost a tooth or teeth due to periodontal disease, an injury, or some other reason.
TYPES OF DENTAL IMPLANTS
- Endosteal (in the bone): This is the most commonly used type of implant. The various types include screws, cylinders or blades surgically placed into the jawbone. Each implant holds one or more prosthetic teeth. This type of implant is generally used as an alternative for patients with bridges or removable dentures.
- Subperiosteal (on the bone): These are placed on top of the jaw with the metal framework's posts protruding through the gum to hold the prosthesis. These types of implants are used for patients who are unable to wear conventional dentures and who have minimal bone height.
The ideal patient for a dental implant should have good general and oral health. Adequate bone in the jaw is needed to support the implant. The best patients for implants are those with healthy gum tissues that are free of periodontal disease. X-rays and CBCT are used for treatment planning for implants.
Implants are not recommended for
- Smokers
- People who have autoimmune diseases or take medicines used for these conditions
- People who have had radiation therapy to the head and neck
- People with uncontrolled diabetes
This procedure is a team effort between the patient, dentist and the implantologist. The implantologist and dentist will consult with the patient to determine where and how the implant will be placed. Depending on the patient’s specific condition and the type of implant chosen, implantologist will create a treatment plan tailored to meet the patient’s needs.
Implant placement can be a single step or two-step procedure.
- Replacing a Single Tooth: If a single tooth is missing, one implant and a crown can replace it.
- Replacing Several Teeth If several teeth are missing, implant-supported bridges can replace them.
- Replacing All of Your Teeth: If all teeth are missing, an implant-supported full bridge or full denture can replace them.
- Sinus Augmentation: A key to implant success is the quantity and quality of the bone where the implant is to be placed. The upper back jaw has traditionally been one of the most difficult areas to successfully place dental implants due to insufficient bone quantity and quality and the close proximity to the sinus. Sinus augmentation can help correct this problem by raising the sinus floor and developing bone for the placement of dental implants.
- Ridge Modification Deformities in the upper or lower jaw can leave with inadequate bone in which to place dental implants. To correct the problem, the gum is lifted away from the ridge to expose the bony defect. The defect is then filled with bone or bone substitute to build up the ridge. Ridge modification has been shown to greatly improve appearance and increase chances for successful implants that can last for years to come.
WHAT CAN I EXPECT AFTER RECEIVING A DENTAL IMPLANT?
Dental implants are like our own teeth and will require the same care. In order to keep the implant clean and plaque-free, brushing and flossing still apply.
After treatment, your implantologist and dentist will work closely to develop the best care plan for you. Periodic follow-up visits will be scheduled to monitor the implant, teeth and gums to make sure they are healthy.
Implant Materials: Implants are made of titanium which is biomedical grade and is considered as gold standard. Various brands are available based on the designs, shape and size. Types will be discussed and choice will be given to the patients.
Problems also can develop years after implants are placed. For example, just like natural teeth and gum tissue, the gum around implants can become infected by bacteria. This leads to a form of periodontal disease called periimplantitis. If left untreated, this condition can cause bone loss. Then the implant can become loose and have to be removed. Generally, this situation can be treated in a way very similar to treatments for periodontal disease affecting natural teeth.
Implant placement will be followed by restorations by the prosthodontist (after 4 weeks – 12 weeks) for placement of crown, bridge or dentures.

Periodontology/periodontics is the specialty of dentistry that studies supporting structures of teeth (gingival – the gum, bone) as well as disease and condition that affect them. Periodontist is the dentist who specializes in periodontology.
ORAL PROPHYLAXIS
Oral prophylaxis is cleaning of the teeth by a dentist or dental hygienist, including removal of plaque, calculus, and extrinsic stains; done as a preventive measure for control of gingivitis.
It's recommended to get prophylaxis at least every six months, and patients with periodontal disease should have it every three to four months.
It is usually single visit but in severe stains/tartar may need two visits.
We recommend brushing, flossing and swishing with mouth rinse twice a day—morning and night before bed.
CURETTAGE
Curettage is a deep cleaning process that includes scraping the tartar off the teeth above and below the gum line and planning or smoothening the tooth at the root. Curettage usually needs two visits.
CROWN LENGTHENING
Crown lengthening is a surgical procedure performed by a dentist, or more frequently a specialist periodontist. There are a number of reasons for considering crown lengthening in a treatment plan. Commonly, the procedure is used to expose a greater amount of tooth structure for the purpose of subsequently restoring the tooth prosthetically. However, other indications include accessing subgingival caries, accessing perforations and to treat aesthetic disproportions such as a gummy smile. There are a number of procedures used to achieve an increase in crown length. Depending on the teeth involved, visits may vary from 1 to 4 visits.
GINGIVECTOMY
Gingivectomy is a dental procedure in which a dentist or oral surgeon cuts away part of the gums in the mouth (the gingiva). By removing the pocket wall, gingivectomy provides visibility and accessibility for complete calculus removal and thorough smoothing of the roots, creating a favourable environment for gingival healing and restoration of a physiologic gingival contour.
Techniques
Gingivectomy can be performed by various techniques.
- Surgical gingivectomy
- Gingivectomy by electrosurgery
- Laser gingivectomy;
In case of full mouth, gingivectomy may need two visits.
FLAP SURGERY
Gingival flap surgery is a procedure in which the gums are separated from the teeth and folded back temporarily to allow a dentist to reach the root of the tooth and the bone. Gingival flap surgery is used to treat gum disease (periodontitis). It may be recommended for people with moderate or advanced periodontitis, especially if the initial, non-surgical treatment (scaling and root planing) has not eliminated the gum infection. It may also be done in conjunction with another procedure known as osseous (bone) surgery.
The dentist will first remove all plaque and tartar (calculus) from around your teeth and make sure that the oral hygiene is good. Before flap surgery, the periodontist will determine whether the general health or your current medications allow for a surgical procedure to be carried out.
After numbing the area with a local anaesthetic, scalpel will be used to separate the gums from the teeth and then lift or fold them back in the form of a flap. This gives direct access to the roots and bone supporting the teeth. Inflamed tissue is removed from between the teeth and from any holes (defects) in the bone. Then scaling and root planing will be performed to clean plaque and tartar. If there are bone defects, osseous recontouring can be done to eliminate them, which smoothes the edges of the bone using files or rotating burs.
After these procedures are completed, the gums will be placed back against the teeth and anchored in place using stitches. If it is resorbable stitches, it will dissolve on its own, if not it has to be removed in a week to 10 days by the dentist after the surgery. The surgical site will be covered with an intraoral bandage known as a periodontal pack or dressing.
Depending on the gum region, either full mouth or quadrant, visits may vary from one to four.
Follow-Up
There will be mild-to-moderate discomfort after the procedure, but pain medications would be prescribed to control it.
The patient may have some swelling, and this can be minimized by applying an ice pack to the outside of your face in the treated area. In some situations, antibiotics may be prescribed to prevent an infection, and these should be taken as instructed. A followup will be done in a week to 10 days.
It is very important to keep the mouth as clean as possible while the surgical site is healing. Should brush and floss the rest of the mouth normally. If the surgical site is not covered by a periodontal pack, toothbrush can be used to gently remove plaque from the teeth. Antimicrobial mouth rinses containing chlorhexidine are commonly prescribed following periodontal surgery. Although these rinses do not remove plaque from the teeth, they kill bacteria and help the mouth to heal.

Orthodontics is a specialized branch of dentistry that focuses on prevention as well as treatment of misalignment of teeth. Orthodontic treatment is a way of straightening or moving teeth, to improve the appearance of the teeth. It can also help to look after the long-term health of your teeth, gums and jaw joints, by spreading the biting pressure over all your teeth.
An orthodontist is a dentist who specializes in orthodontic treatment.
Many people have crooked teeth or gap between teeth which can lead to difficulty in speech and also difficulty in maintain teeth clean and also gives unesthetic appearance. Orthodontic treatment will straighten the teeth and move them into a better position. This can improve their appearance and the way the teeth bite together, while also making them easier to clean.
Some people have upper front teeth that stick out and look unsightly. These 'prominent' teeth are more likely to be damaged, with orthodontic treatment we can move the teeth back into normal position. When the teeth don't meet correctly, this can put strain on the muscles of the jaw, sometimes cause headaches and leads to jaw and joint problems (TMD). Orthodontic treatment can improve the bite more evenly and reduce the strain. The best time to get a child for orthodontic evaluation is at the age of 7 because this is the time when the new teeth erupts and after evaluating the teeth necessary treatment can be done to prevent any severe problem in future. During this periods the eruption and formation of teeth are monitored. Later if the teeth are still not in the right place after eruption of all permanent teeth full braces are fixed for orthodontic correction. But adults can also have orthodontic treatment to improve facial appearance. Age is less important than having the right number of teeth.
STEPS FOLLOWED IN ORTHODONTIC TREATMENT:
The most important thing is to have a full examination.
1. Records will be taken in first appointment which serves as a tool for the orthodontist to plan the treatment. This will usually involve looking at your teeth, taking photos and dental x-rays and taking impression for making plaster models of your teeth.
2. Orthodontist will then discuss what treatment is possible. Treatment varies according to individual patient’s requirement. Some may require few permanent teeth to be taken out to create space for alignment. Once you are sure you want to go ahead, the treatment can be started.
3. Then the appliance is fixed, this is an active phase. Appliance is periodically adjusted to move teeth into proper position. - The length of treatment depends on how severe the problem is, and it may take anything from a one to two-and-a-half years. Most people can be treated in one to two years.
4. Finally after treatment – Retention phase starts during which patient is required to wear a retainer so that teeth retain their new position.
Types of Appliances
- Removable braces:
Simple treatment may be carried out with a removable brace (a plate that can be taken out to be cleaned). It has delicate wires and springs attached, which move the teeth using gentle pressure. - What is a fixed brace?
Often, teeth need to be guided more accurately than they can be using a removable brace. So a fixed brace is used. This has brackets and bands which are temporarily stuck to the teeth. A flexible wire joins all the brackets and allows the teeth to be moved. You can't take the appliance out yourself, so it is called a fixed appliance. There are 3 types of braces – Metallic, Ceramic and Invisalign. - What is a functional brace?
It is sometimes possible to change the way the jaws grow, using a functional brace. This works by using the power of your jaw muscles and can help with certain types of problem. - What are 'invisible braces'?
They are tough, clear plastic 'aligners' (moulds) that are used to straighten teeth. Several sets of specially moulded, slightly different aligners are made for each patient. Each set is worn for 2-3 weeks before being replaced with the next one. They are made from clear plastic, so they are nearly invisible. This means that no one need know you are straightening your teeth. The aligners should be worn for 22 to 23 hours a day for the best results. They can be easily removed for eating, drinking, brushing, and for cleaning in between your teeth. You need to have all your adult teeth before you can have this treatment.
Treatment Duration
Most patients wear braces for 1-1/2 to 2 years. However, the length of time in braces can vary greatly for each person based on growth, the severity of the problem, and how well the patient takes care of their braces and keeps up their oral hygiene.
Follow-Up
Frequent follow-ups or "adjustments" are needed to replace worn-out rubber bands, check on your teeth's progress, and make adjustments to the wires to make sure teeth are being pulled in the right direction.
At Mig Dental, we usually recommend follow up every 4-5 weeks. The orthodontist will replace the elastic bands on each bracket and may also take out and replace the wire. Each adjustment should take not more than 20 minutes.
Skipping follow-ups can hinder progress, and may cause you to need braces for a longer period of time.
Ortho Instructions
GENERAL INSTRUCTIONS FOR BRACES & ORTHODONTIC TREATMENT
Braces & Orthodontic Treatment are done to align crooked teeth, irregular bites and close gaps between teeth. Both children and adult might need an orthodontic treatment and it is necessary to follow these instructions to get the best results in the time period prescribed.
- Your appliance is fixed to your teeth and cannot be removed until the end of treatment.
- Some discomfort may occur during the first few days.
- Special attention must be paid to oral hygiene as your fixed appliance will make it more difficult for you to keep your teeth and gums clean.
- You must continue to have routine dental inspections throughout your orthodontic treatment. If it becomes essential to change your next appointment, please let us know as soon as possible. Frequent delays make a good result unlikely.
CLEANING:
- Brush your teeth and braces with orthodontic tooth brush at least three times a day (and always after eating).
- Change your brush every month.
- Clean between your teeth using Interdental brush.
- Use quality toothpaste Toothpastes containing fluoride have been proven to help prevent cavities.
- Use a fluoride mouthwash to help reduce the risk of cavities.
- Floss regularly and thoroughly
- Have your toothbrush and floss with you at all times so that you can clean your teeth even when you are not at home.
EATING:
- You must be careful with what and how you eat. You must avoid anything too hard or sticky i.e. toffees, chewing gum, crusty bread, nutty breakfast cereals and hard biscuits.
- From now on all food, even things you think are soft, must be cut up first into small pieces and chewed gently on your side teeth.
- Most of this is common sense but remember to think before you eat something.
- A breakage can put treatment time back and mean that your braces will be on longer than necessary.
PROBLEMS:
- After your brace has been fitted your teeth will feel tender, this is normal.
- In case of pain: Please take one pain reliever like paracetamol
- If brackets or bands rub your lips and cheeks you may need to use brace relief (wax)
- In case of ulceration: Please apply prescribed ointment
BREAKAGES:
- Try not to break your brace - remember breakages mean longer treatment.
- If you break your brace and/or if that come off, always keep it safely and bring any loose bands and any broken pieces with you to your appointment. Please ring immediately and get an appointment unless your next appointment is within a day or so.

Zoom is a bleaching process. It is in-office tooth whitening procedure using Zoom Advanced Power Chairside Lamp.
Bleaching is done to lighten discoloration of enamel and dentin.

Surgical Removal of an Impacted Third Molar (Wisdom Tooth)
Impacted Tooth
An Impacted tooth is one that has failed to erupt in to its normal position beyond its age of eruption.
A tooth gets impacted due to various reasons, the most common being lack of availability of space for its eruption
Impacted Third Molar (Wisdom Tooth)
The most common tooth that gets impacted is the third molar, also called as wisdom tooth. Third molars are the last teeth to erupt, around the age of 18 to 25, ending up in lack of space to erupt. Impacted third molars cause pain, swelling, difficulty in mouth opening and chewing, cyst formation etc and therefore require removal of the tooth.
Impacted Tooth Removal
Unlike removal of an erupted tooth, impacted tooth needs a minor surgical procedure for its removal. Impacted tooth needs a thorough pre-operative evaluation, which includes clinical and radiographic assessment.
Clinical assessment includes
- evaluating the medical history and overall medical status of the individual
- evaluating mouth opening and visualization of the tooth
- presence of infection
- evaluation of gums and bone covering the tooth
- angulation of the impacted tooth
Radiographic assessment includes
- evaluating the bone covering the tooth
- relationship of the adjacent tooth
- relationship of the nerve underlying the tooth
At Mig Dental, we do a careful clinical assessment and then an Orthopantamogram (OPG) is obtained. The OPG gives a 2 dimensional view of the impacted tooth. If there is close approximation of the tooth to the underlying nerve, this may not be seen on an OPG. These types of impacted teeth need a Cone-Beam Computed Tomography (CBCT) assessment which is available at the centre itself.
The position of the impacted tooth, the procedure and the postoperative care will be explained to the patient and informed consent will be obtained.
The procedure is usually done under local anaesthesia. The surgical procedure involves incising the gums and clearing the bone covering the impacted tooth to visualise it. The tooth is gently elevated out. Sutures are then placed to close the surgical site.
Depending on the severity of the impaction and anxiety of the patient, sometimes general anaesthesia and sedation are used.
The After Effect
All instructions to be followed after the tooth removal will be explained to you. We prescribe as minimal medicines as possible. This includes a potent anti-inflammatory analgesic and if required an antibiotic. The anti-inflammatory drug would take care of the pain and the inflammatory sequelae. However, there could be swelling over the operated site due to the body’s response to the procedure. This would settle down in 2-3 days. Usually a review is done 5-7 days after the procedure, during which the sutures will be removed.
Post Extraction Instructions
1. Continue biting on the cotton for 30 minutes following the procedure and then throw the cotton.
2. Can have soft food or room temperature drinks after an hour. Please avoid hot drinks/food for the rest of the day.
3. DO NOT - spit, rinse, suck using straw, smoke, drink carbonated or alcoholic beverages for at least 24 hours. (The goal is to keep blood clot in the socket to prevent bleeding).
4. No massage or hot compresses application unless advised.
5. Brush gently the next day and gentle lukewarm salt water rinse can also be used to freshen your mouth.
6. Take the prescribed medications as directed.
7. If sutures were applied, follow in five days for removal as instructed.
8. Follow up appointment for review as scheduled.
If any other queries, kindly call us
